Maxillofacial Surgery
Hair Transplant
Hair transplant surgery is a procedure that redistributes hair follicles from a donor site, typically the back or sides of the scalp, to areas experiencing hair loss or thinning. It’s a permanent solution for male pattern baldness and certain types of hair loss in women. Techniques like Follicular Unit Transplantation (FUT) involve removing a strip of scalp for donor follicles, while Follicular Unit Extraction (FUE) harvests individual follicles directly. Both methods ensure natural-looking results with minimal scarring. Recovery time varies, but patients typically resume normal activities within a few days. Consultation with a qualified surgeon helps determine the best approach based on individual needs.







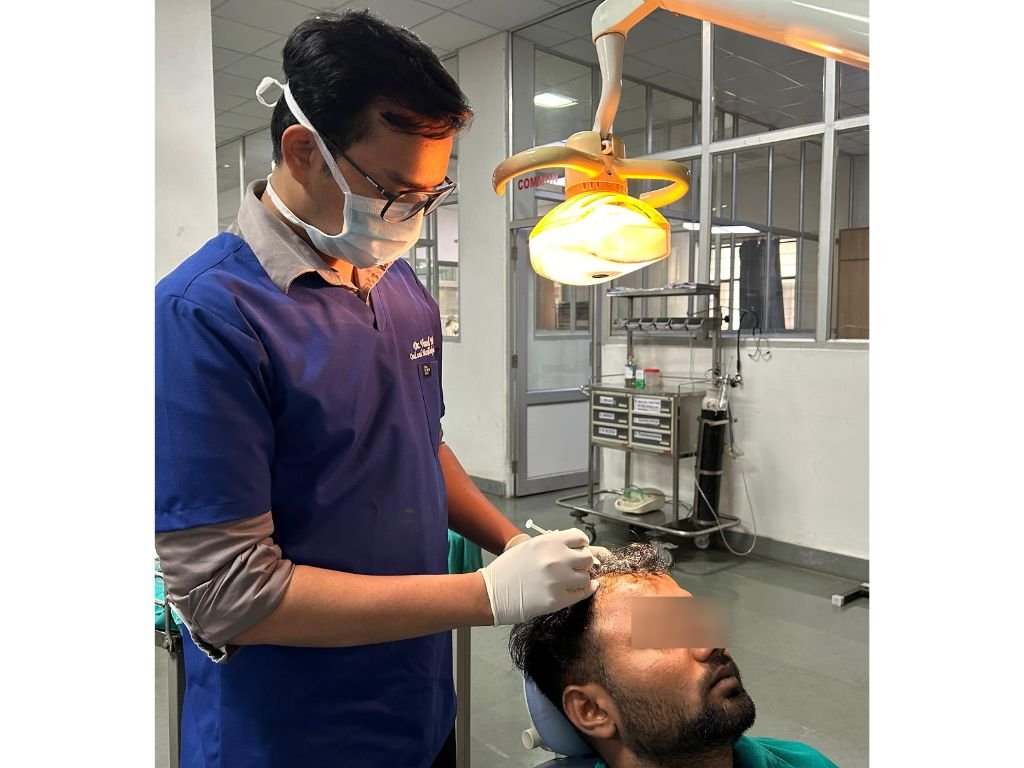
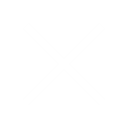
HAIR PRP
Platelet-Rich Plasma (PRP) therapy for hair involves drawing a patient’s blood, processing it to concentrate platelets, growth factors, and cytokines, and injecting this into the scalp. PRP stimulates hair follicles’ activity, promoting hair growth and thickening. It’s a non-surgical, minimally invasive treatment for various types of hair loss, including male and female pattern baldness. The procedure typically requires multiple sessions over several months for optimal results. PRP is considered safe with minimal side effects, such as temporary swelling or mild discomfort at injection sites. Results vary, but many patients experience improved hair density and quality over time.
FACE PRP
Platelet-Rich Plasma (PRP) therapy for the face involves using the patient’s own blood plasma, enriched with platelets and growth factors, to rejuvenate skin and improve texture. After drawing blood, the PRP is separated and injected into specific areas of the face or applied topically after microneedling. PRP stimulates collagen production, enhances skin elasticity, and reduces fine lines and wrinkles. It’s a natural approach to facial rejuvenation, promoting a youthful appearance with minimal downtime. Multiple sessions may be recommended for optimal results, depending on individual skin concerns. PRP for the face is generally well-tolerated, with mild swelling or redness as common temporary side effects.







Facial Plastic Surgery - Nasal Reconstruction
Implant in the healed Extraction site, Implant in the immediate Extraction site with different types of Bone Grafts, Implant associated Complications management.
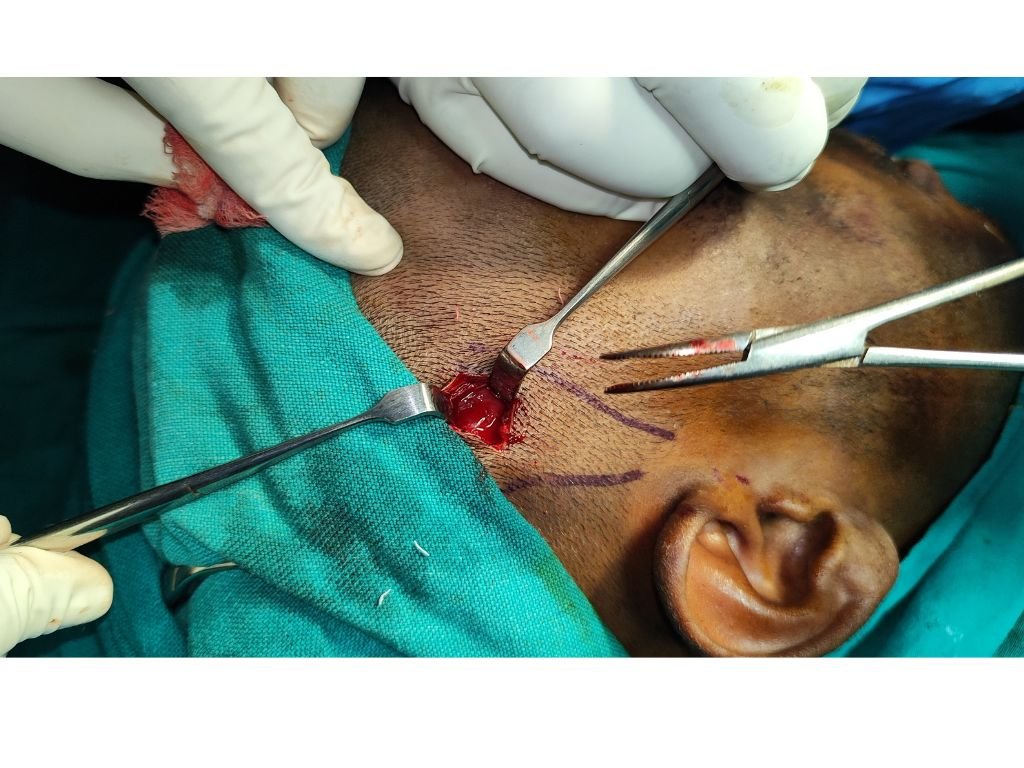
Tracheostomy
An emergency procedure every Maxillofacial Surgeon should be well versed with, is Tracheostomy. A procedure to gain access to airway in both elective and emergency situations, tracheostomy can be done under local anesthesia. Horzontal Incision gives more esthetic result and vertical incision allows faster surgery. After sharply dissecting through skin and superficial fascia, the key to a good tracheostomy is to remain in the midline. Midline provides a relatively avascular plane and prevents potentially life threatening complications like false intubation, injury to oesophagus and Neurovascular complications













Skin Grafting
Excision defects of mucosa may result after surgical treatment of lesions like Leukoplakia, Erythroplakia, Erosive Lichen Planus. If small, they may be closed primarily, otherwise the options include Collagen membrane dressing, Plancental membrane dressing, Split thickness skin graft and local flaps.
Anterior surface, medial surface, lateral surface of Thigh are good donor sites for Split thickness Sking Graft. Since the cheek mucosa is mobile, quilting is recommended. An alternative (not prefered by us) is to use a bolus dressing tied over the the graft securely.
Internal Derangement
Internal derangements of TMJ frequently reach a point where the articular disc cannot be salvaged due to advanced degenerative changes and require Disectomy with or without condylar shave. TMJ can be approached through various incision like preauricular and its modifications, endauricular, postauricular, retromandibular, Rhytidectomy etc. Protecting the facial nerve is the prime consideration. Incision through the capsule close to the lateral lip of artcular fossa reveals the superior joint space. The disc can be reconstructed with temporalis muslce/fascia, cartilage graft or alloplasts. Temporalis muscle/fascia is a reliable donor source and doesn’t have the problem of extrusion as is sometimes seen with alloplastic materials










Eagle's syndrome
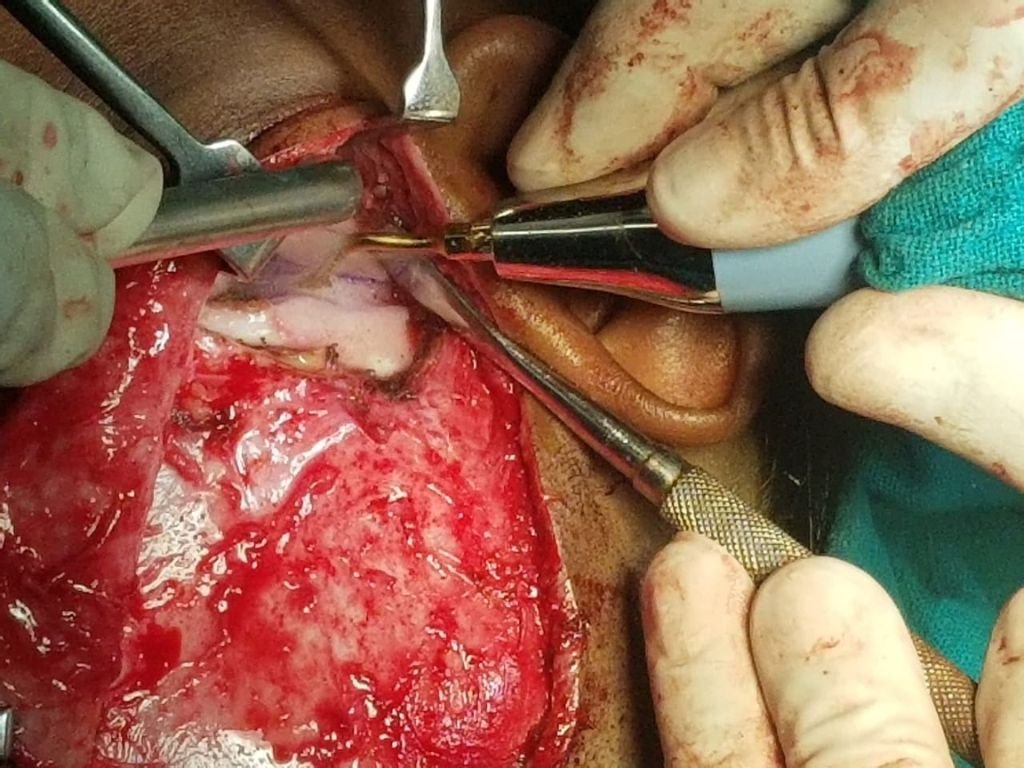
Eagle’s syndrome is primarily managed surgically by styloidectomy. Intraoral Styloidectomy is preferred as it avoids a submandibular scar. However, when it has to be combined with submandibular gland resection, an extraoral approach is preferred. A submandibular incision 2 cm below lower border of mandible through skin and platysma is given. Marginal mandibular nerve must be preserved. Anterior belly of digastric is identified and traced back to posterior belly. Retracting the posterior belly down reveals styloid process.
Submandibular gland can be removed with or without ligating the facial artery. Hypoglossal nerve and Lingual nerve must be preserved.
Oral Squammous Cell Carcinoma
Oral Squammous Cell Carcinoma Primarily spread to Neck lymph nodes, therefore, their management frequently requires neck dissection along with wide excision of the tumor. Neck dissection can range from Supraomohyoid Neck dissection to Radical Neck Dissection. However, current research is more in favour of Modified Radical Neck Dissection which preserves Spinal Accessory Nerve, Internal Jugular Vein and Sternocleidomastoid. Some of the factos that affect the decision are the tumor size, location, histological variant, possibility of followup, possibility of multimodal therapy etc. Mc Fee incision gives a good exposure combined with safety of cover on the carotid furcation.











Eminectomy
Eminectomy is one of the surgical modalities of treatment of Recurrent or Long standing TMJ Dislocations. The joint is accessed through Preauricular or Endauricular or Post auricular approach. The incision is made through skin and superficial fascia The superficial layer of deep temporal fascia is incised. Disssecting between the two layers of deep temporal fascia saves the facial nerve branches. A periosteal incision exposed the articular eminence. A slightly inferiorly directed eminence osteotomy completes the eminectomy. Layered closure of the wound is necessary.
Dental Implants
Dental Implants have become the mainstay of management of edentulism with many advantages over the conventional prosthesis. An implant supported prosthesis may take various forms like implant supported bridge, implant and tissue supported overdenture, implant supported overdenture and the All-on-four concept.







ARTHROCENTESIS
Arthrocentesis is a medical procedure involving the removal of fluid from a joint space using a needle and syringe. It’s performed to diagnose and treat various joint-related conditions such as arthritis, infections, or crystal-induced arthritis (e.g., gout). The procedure helps relieve pain and swelling by draining excess fluid and reducing pressure within the joint. Arthrocentesis also allows for analysis of the joint fluid, aiding in the diagnosis of underlying causes. It’s typically performed under local anesthesia and involves minimal risks, including infection or bleeding. Post-procedure, patients may experience temporary soreness or stiffness but generally recover quickly.
TMJ SURGERY
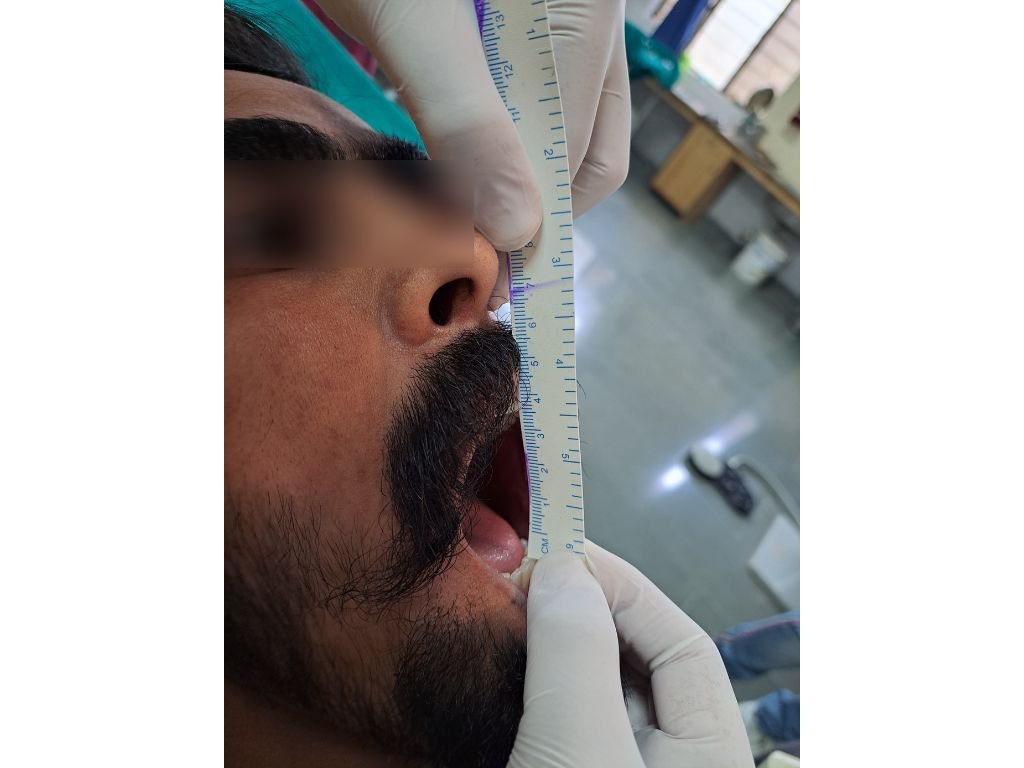
Temporomandibular joint (TMJ) ankylosis surgery addresses a condition where the jaw joint becomes fused, limiting jaw movement and causing pain. Surgical treatment involves separating the fused joint and reconstructing it to restore function. Techniques vary depending on the severity and location of the ankylosis, often involving bone grafts or joint replacement with artificial materials. The goal is to improve jaw mobility, alleviate pain, and restore normal chewing and speaking abilities. Post-surgery, patients undergo rehabilitation to regain jaw function gradually. Risks include infection, nerve damage, or joint stiffness, requiring careful evaluation and skilled surgical management.








SPACE INFECTION
Space infections are deep-seated infections in anatomical spaces, like those in the head and neck. Hilton’s method, named after John Hilton, involves making strategic incisions to drain these infections. This technique aims to release built-up pus and alleviate pressure, reducing the risk of further complications like tissue damage or spread of infection. It’s crucial for managing conditions such as Ludwig’s angina or deep neck abscesses promptly to prevent airway compromise and systemic infection. Modern approaches may incorporate imaging for precise localization and minimally invasive procedures, ensuring effective drainage and optimal patient outcomes.
Neurectomy
Neuralgia is a condition characterized by sharp, shooting, or burning pain along the path of a nerve. Neurectomy is a surgical procedure where a portion of a nerve is removed to alleviate severe or chronic neuralgia that doesn’t respond to conservative treatments like medications or injections. This surgery aims to interrupt the pain signals from reaching the brain, providing relief. Neurectomy is often considered for conditions such as trigeminal neuralgia or occipital neuralgia when other treatments fail. Risks include numbness or sensory loss in the affected area. Careful patient selection and evaluation by a specialist are crucial for successful outcomes.











Orthognathic Surgeries
Orthognathic surgeries aim to correct the deformities of the face. Bilateral Sagitttal Split Osteotomy (BSSO) is one of the most frequently employed procedures to correct mandibular deformities.
Calverial Bone Graft
Calverial grafts are harvested from the parietal bone to reconstruct various bony deformities of face. The presented case involved reconstructing a post-traumatic deformity of frontal bone with Calverial Bone Graft. Exposure of the site was done through bicoronal flap.










TRAUMA
Maxillofacial trauma refers to injuries affecting the face, jaw, and surrounding structures due to accidents, assaults, or sports injuries. Management involves a multidisciplinary approach, including oral and maxillofacial surgeons, plastic surgeons, and otolaryngologists. Immediate evaluation assesses airway patency, bleeding control, and fracture stabilization. Treatment may include surgical repair of fractures, wound closure, and dental rehabilitation. Imaging such as CT scans assists in diagnosis and surgical planning. Postoperative care focuses on monitoring for complications like infection or malocclusion. Rehabilitation often involves physical therapy for facial muscle function and psychological support for patients recovering from facial trauma.
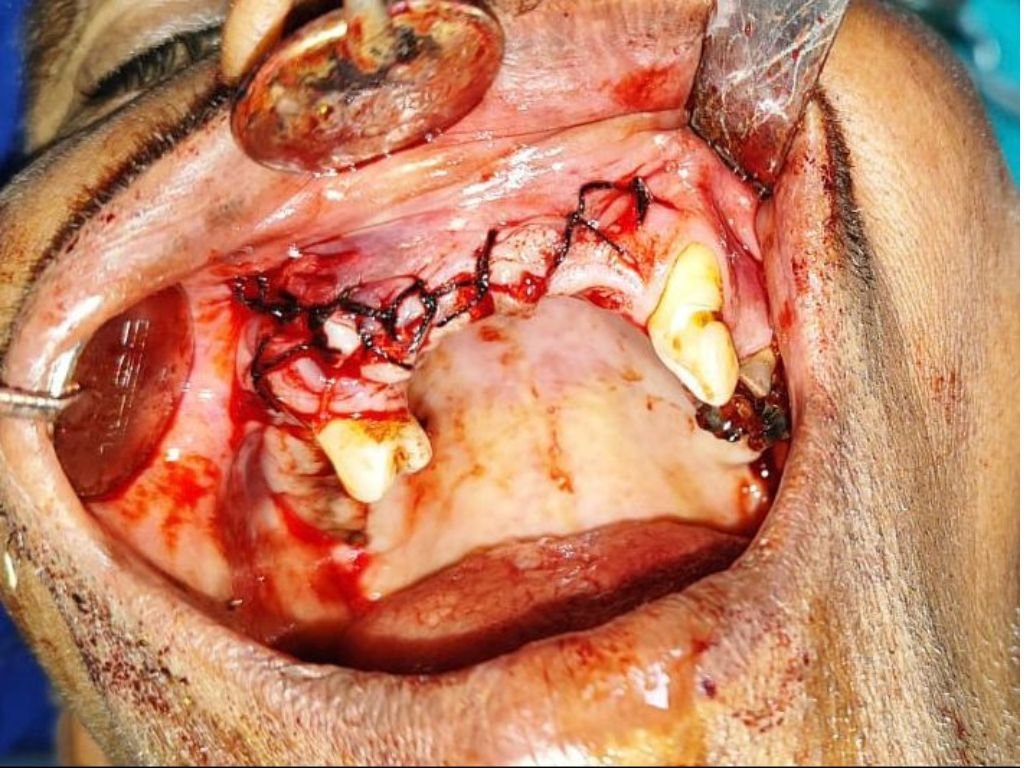
EXTENSIVE PATHOLOGY
Pathology encompasses the study of disease processes, examining structural and functional changes in tissues and organs. It identifies causes, mechanisms, and consequences of abnormalities, crucial for diagnosis and treatment. Divided into anatomical (macroscopic and microscopic) and clinical pathology (laboratory analysis), it aids in understanding disease origins, progression, and outcomes. Pathologists interpret biopsies, autopsies, and laboratory tests to diagnose conditions ranging from infections to cancers. Through research, pathology advances medical knowledge, guiding therapeutic interventions and public health strategies. It underscores the importance of detailed examination and analysis in medicine, crucial for improving patient outcomes and shaping healthcare practices worldwide.